Research Priorities for the Growing Population of Childhood Cancer Survivors

Regardless of political affiliation, most cancer survivors can agree that the specific concerns of survivors received little attention during the presidential campaign. With the election now over, NCCS is inviting cancer survivors from around the country to highlight those specific needs, and propose a cancer care and research agenda to the new Administration and the new Congress.
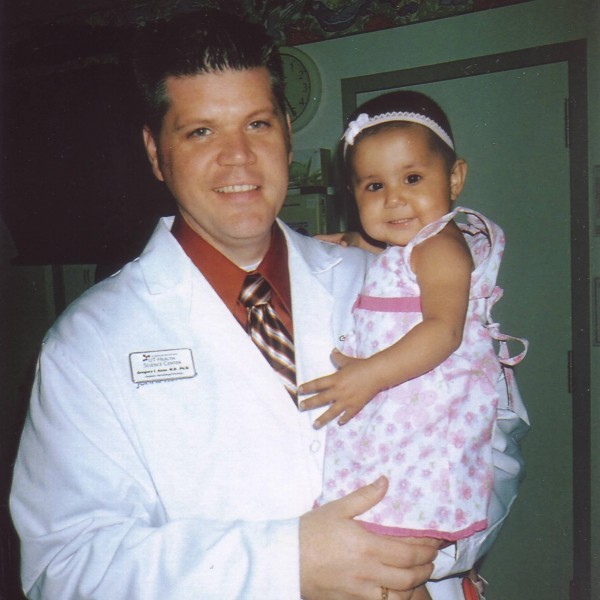
Post by Greg Aune, MD, PhD
@gregoryjaune
Cancer is most certainly not a Republican or Democratic issue, yet solving the challenges facing cancer patients in the United States will require ongoing collaboration from our newly elected executive administration and the 115th Congress. Going forward, it is imperative that we continue to capitalize on the recent momentum established by the National Cancer Moonshot and other evolving collaborative efforts in the cancer research and clinical care umbrellas.
Pediatric cancers include an array of biologically unique cancers that are rare and many are exclusively seen in children. For these diseases, it is imperative that we continue to study the scientific underpinnings of these cancers and use that knowledge to develop novel, targeted less toxic therapies. But, it is becoming clear that the development of novel therapies for pediatric cancers is not by itself likely to solve the problems faced by the growing numbers of childhood cancer survivors.
Because the development of new drugs for pediatric cancers lags behind efforts in adult cancers, it is additionally important to invest in new research areas that focus on perfecting the administration of our existing chemotherapy and radiation regimens. Currently, there is a dearth of knowledge pertaining to the effects pediatric chemotherapies and radiation have on normal organs such as the heart, brain, liver, and kidneys.
Survivors of childhood cancer are a growing population that is expected to number 500,000 in the United States by 2020.[1] This growing number is the product of steadily increasing 5-year survival rates for childhood cancer that began in the 1940s when Sidney Farber first introduced systemic chemotherapy to the anticancer armamentarium.
In the first decade of the 21st century, epidemiologic evidence began to emerge confirming what was long expected—that curative regimens for childhood cancer are associated with tremendous long-term cost and increased risk of severe morbidity and mortality. Numerous analyses from childhood cancer cohorts in the United States and Europe have highlighted the shortcomings of successful childhood cancer therapy.
In the United States, the Childhood Cancer Survivor Study (CCSS) has served as a central resource to quantify the health problems faced by childhood cancer survivors. Analyses of outcome data collected from over 34,000 long-term survivors have clearly established a link between childhood cancer therapy and an increased risk of severe health effects including secondary cancers, cardiovascular disease, strokes, endocrinopathies, infertility, neurocognitive deficits, and pulmonary diseases. More important are the numerous studies that have clearly shown that long-term survivors of childhood cancer have a markedly increased mortality rate when compared to age-matched control groups.
Our new leaders must understand that the plight of childhood cancer survivors has become a major priority with patients and their families. With increasing numbers of children surviving their cancer, the devastating long-term consequences of successful treatment are now quantified. A recent study of survivorship patient cohorts indicated that by age 50, 60% of childhood cancer survivors will be either dead or suffering from a life-threatening health complication caused by their pediatric cancer therapies.[2]
As our new leaders begin to set their policy priorities, it is important to highlight critical research areas that have the potential to improve the quality of life for childhood cancer survivors. With this in mind, I would like to identify three broad research areas that I believe, if funded and expanded, would lead to an overall healthier population of childhood cancer survivors.
We must develop and emphasize:
- Preclinical laboratory models of cancer survivorship. – The bulk of our knowledge in health outcomes for childhood cancer survivors has been obtained from retrospective cohort studies that have largely focused on correlating specific treatment exposures with the development of specific health problems later in life. Thus, we currently have minimal knowledge that details how chemotherapy and radiation damage normal tissues and lead to late effects. While efforts to develop targeted less toxic therapies are ongoing, in the near term this strategy is unlikely to eliminate our use of the current curative regimens. Therefore, going forward, it is vital that we develop robust preclinical research models to address this major gap in our oncology research portfolio.
- Research exploring the premature aging phenotype observed in many childhood cancer survivors. – There is emerging evidence that suggests survivors of childhood cancer age prematurely. Several studies of survivor cohorts have documented elevated risks of age-related conditions such as cardiovascular disease, secondary cancers, and possibly dementia. The biological basis of these epidemiologic observations is mostly unknown. Thus, we must invest in research that is aimed at understanding how early chemotherapy and radiation exposure alter normal aging processes in long-term survivors.
- Applying precision medicine concepts to late treatement-induced toxicities. – With the announcement of the Pediatric MATCH (Molecular Associated Therapy Choice) Trial, efforts to harness the promise of genomic sequencing to deliver tumor-targeted therapy for pediatric cancers have moved to the forefront. These efforts are largely focused on utilizing rapid sequencing technology to identify targetable mutations in pediatric cancers and thereby deliver treatments targeting these changes within an individual patient’s tumor. In contrast, the same sequencing technology can be utilized to identify the underlying germline background that mediates how an individual patient responds to standard chemotherapy regimens and results in toxicities. Studying our current range of pediatric cancer therapies from this perspective must be systematically and prospectively initiated in all new childhood cancer patients.

Video: Dr. Greg Aune Describes His Treatment Experience »
“I think my story kind of makes people take pause.”
Researchers, clinicians, patients, families and advocates must continue to diligently pursue a new day in cancer care—one where curative regimens are available for all childhood cancers and all survivors are living a life free from health problems caused by successful cancer treatment. Our new leaders have the power to make this day a reality.
About the Author
Gregory J. Aune, MD, PhD, is a 25-year survivor of Hodgkin’s Lymphoma. He is a policy advisor for NCCS, a St. Baldrick’s Foundation Scholar, and the Stephanie Edlund Distinguished Professor in Pediatric Cancer Research at Greehey Children’s Cancer Research Institute in San Antonio, TX.
Twitter: @gregoryjaune
Website: https://ccri.uthscsa.edu/GAune.html
Research Gate: www.researchgate.net/profile/Gregory_Aune
The views & opinions expressed in any guest post featured on our site are those of the guest speaker and do not necessarily reflect the opinions & views of the National Coalition for Cancer Survivorship. Read our blog and comment policies here.