Guest Blog: Improving How Doctors and Patients Have Difficult Conversations

Post by Cristian Zanartu, MD
Montefiore Einstein Center for Cancer Care
Bronx, NY
As humans we are challenged with this disease as old as our chromosomes, struck at the core of our identity, of our body, of our sense of self. We are removed from work, from a normal agenda, from our families, from our mirrors. We learn to fight with something inside of us. We learn to split ourselves apart.
However, there is one part of ourselves that can always be preserved, always untouched, always whole: our dignity. Time and again studies show that dignity—defined in a multiplicity of ways—is one of the main elements that help patients cope with serious or advanced disease. Dignity has been linked to quality of life, symptom control, and even survival. Dignity can help patients engage to surmount challenges, like days filled with hours of chemotherapy. Dignity can help confront news when they are not as expected. Dignity can be the distinguished silence with which patients assertively prepare for their passing, and become examples of bravery and acceptance for their loved ones.
As a palliative medicine specialist, I see that one of the main hazards for patients’ dignity is lack of communication. Well-intended families and doctors protect patients from real discussions about what to expect from their treatments. This is particularly frequent of those cancers with poor prognosis and when therapies with only limited benefit are being offered.
The Help-Hurt Tool

Dr. Zanartu Demonstrates the Help-Hurt Tool (click to expand)
The logic behind this tool is quite simple: every single treatment in medicine—whether it be an over-the-counter tablet of 100 milligrams of aspirin or open-heart surgery—possesses a potential benefit and a potential risk. Cancer treatments of course don’t escape this.
In regards to benefit, some cancer treatments provide promise of cure—like chemotherapy regimens for many malignancies originating from blood cells or for initial stages of some organ cancers. On the other hand, some cancer treatments offer only some more time of survival without growth of the disease, therefore extending life and improving symptoms, but not a cure. This time can be estimated in years, months or, sadly, just in weeks. And in some instances, a cancer treatment is just a desperate attempt at “trying something else,” either at the persistence of patient and family, as a source for hope or as an understandable—yet not frequently justified—need for a doctor to send his patient a message of non-abandonment.
Read the Companion Post
Ms. M is an 81-year-old woman with Stage IV Pancreatic Cancer. She had remained in great health until her recent diagnosis, after which her energy had plummeted…The ways cancer treatments can harm also vary significantly. For instance, drugs like hormonal blocking agents seldom produce dangerous side effects. On the other hand, chemotherapy infusion drugs like Cisplatin can be difficult to tolerate and lead to more side effects. Generally a patient that is older and/or has more medical issues will tolerate these drugs worse than a healthy/young patient.
We do not possess absolutes in prognostication in medicine. We can never be sure how much a therapy will help or hurt a patient. Every so often a frail patient can make a fantastic recovery from an aggressive intervention, and on the other end, a healthy patient dies from the unexpected complication of an otherwise low risk procedure.
But these are of course not the most likely scenarios. In medicine we often know what will be the most likely scenarios, we can talk on averages, a.k.a. the most likely result of a treatment or intervention. But regardless of information being imperfect, don’t patients deserve to know these expectations? Should we leave the knowledge that allows us to know what to expect only at the doctor’s side of the table, and leave patients always in the unexpected? The answer that this proposed tool gives to this question is: no.
How the Tool Works
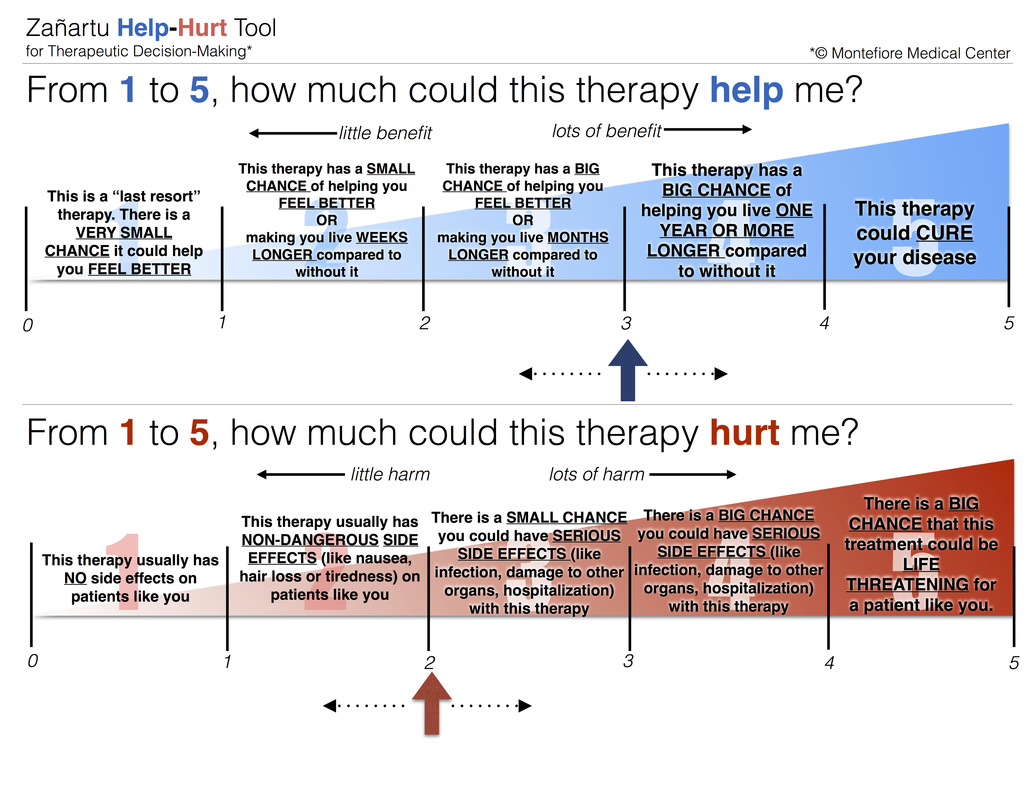
Clinical experience gives doctors the capacity to formulate a judgment. This judgment is usually the result of adding the information provided by evidence-based medicine regarding the usual result of a treatment plus the patient’s known circumstances (old vs. young, frail vs. strong, healthy vs. sick). The Help-Hurt tool offers doctors a chance to express this opinion to their patients. This way patients can become better decision makers, importing the physician’s realistic clinical judgment in a useful way.
The Zanartu Help-Hurt tool, courtesy of Montefiore Medical Center (click to view full-size)
The second scale offers the same logic for expected harms of a therapy, in red. How much could this therapy hurt me? The higher the score, the more harmful the treatment could be. A score of 1 represents a therapy with usually no side effects. A score of 2 represents a therapy with non-dangerous side effects like nausea, hair loss, acne/rash, or headaches. A score of 3 represents a therapy with a small chance of serious side effects like infection, damage to other organs, or other complications requiring hospitalization. A score of 4 represents a big chance of the same serious complications. Finally, a score of 5 represents a therapy that could likely be lethal or life threatening itself.
As you can see, every single possible outcome written on the tool is expressed in chances or probabilities. Again, your doctor will never be absolutely sure of how a treatment will help you or hurt you, but these are the most likely scenarios. By knowing them, a patient can make a better informed-decision.
On the bottom of both scales there are arrows that can be moved over to particular help and hurt scores. That way a particular therapy on a particular patient is given the expected scores on both the help and the hurt scales. If different therapy options are on the horizon, a set of help and hurt scores are given for each therapy. For example, therapy A has a help of 3, but a hurt of 4. Meanwhile, therapy B has a help of 4, but a hurt of 5. Ideally, therapies would have a high help score and a low hurt score. However, that is not always possible in medicine today. Often, as diseases get worse and patients sicker, the help score becomes smaller and the hurt score higher.
Incorporating such reality into the conversation is hard, for both patient and doctor. When confronted with cancer, patients need the comfort of being told things are going to be okay. And okay usually means getting rid of disease. Doctors feel the need to give that message. The expectation is for medicine to make a big difference, to save the day, to save a life. Hopefully this tool will be there to display high help scores and low hurt scores when likely successful plans are being offered. But when this is not case: how can doctors be comfortable saying: “this therapy will help you marginally, this other will help you little, this one might just hurt you a lot.” Doesn’t seem like this is what doctors were trained to say. How do we keep hope while giving realistic information?
The answer to these questions opens a whole other can of worms, one this article is unlikely to resolve. How can we re-frame hope when people don’t get better? Have you ever been to an ICU ward? It has a lot of reality, often times little hope. Can we build a hope that transcends old and young, sick and healthy, death and alive? Can we dare to believe in a hope about who we are? About what we are truly worth? About what we truly mean to the others we have met and loved? When hopes of achieving a cure are lost… can we hope to remain ourselves through the challenge, to keep our light on, to rise to the occasion with a body hurt by disease but a dignity intact?
About the Author
Cristian Zanartu, M.D.—a palliative medicine specialist at Montefiore Einstein Center for Cancer Care—treats patients at all stages of their disease, providing continuous support and care to help relieve their physical and emotional symptoms, while guiding them and their loved ones as they face complex choices and decisions.
Dr. Zanartu’s full bio can be read on the Montefiore Cancer Center’s website.
Read more about the Help-Hurt Tool at www.helphurttool.com.
The views & opinions expressed in any guest post featured on our site are those of the guest author and do not necessarily reflect the opinions & views of the National Coalition for Cancer Survivorship. Read our blog and comment policies here.




