Fall 2022 Cancer Policy Roundtable
NCCS hosted the 22nd Fall Cancer Policy Roundtable (CPR) on November 17, 2022. CPR is a semi-annual meeting convening stakeholders in the cancer community. This year’s Fall CPR featured several engaging sessions:
- Congresswoman Debbie Wasserman Schultz (FL-23) reflected on her personal cancer survivorship journey and discussed her forthcoming survivorship legislation.
- A panel of health policy experts offered their perspectives on the short-and long-term implications of the mid-term elections, with attention to how the election results will affect cancer survivors.
- We heard from our two Stovall Award winners, as they reflect on their careers in medicine and advocacy.
- A panel of experts weighed in on how medical debt impacts cancer survivors, including Noam Levey from Kaiser Health News. Levey shared his findings from Diagnosis: Debt, a reporting partnership between Kaiser Health News and National Public Radio.
- We are also honored that the National Cancer Institute’s new director, Dr. Monica Bertagnolli, delivered the closing keynote.
Sessions
Opening Keynote: Congresswoman Debbie Wasserman Schultz
Florida’s 23rd Congressional District
“Confronting cancer head-on with an all-hands-on-deck approach is a personal and professional mission for me.”
Summary
 In the opening keynote, Congresswoman Wasserman Schultz (FL-23), a champion for cancer survivors and a survivor herself, shared her personal cancer experience and discussed her previous legislative successes that have directly impacted cancer survivors. She asserted, “confronting cancer head-on with an all-hands-on-deck approach is a personal and professional mission for me.”
In the opening keynote, Congresswoman Wasserman Schultz (FL-23), a champion for cancer survivors and a survivor herself, shared her personal cancer experience and discussed her previous legislative successes that have directly impacted cancer survivors. She asserted, “confronting cancer head-on with an all-hands-on-deck approach is a personal and professional mission for me.”
She also revealed exciting news about her forthcoming legislation that will directly benefit cancer survivors. Her comprehensive survivorship legislation, the Comprehensive Cancer Survivorship Act, has already garnered bipartisan support and will be introduced by the end of the year.
“Survivorship,” she said, “like our health system, can no longer be viewed as one-dimensional,” emphasizing the need for a comprehensive approach to helping survivors. Thus, her legislation will address the entire continuum of care to close many of the gaps patients face so that they may no longer feel like they are “lost in transition.” Specifically, it will provide coverage for care planning services to address transition to primary care, develop comprehensive navigation services, establish workforce assistance grants, provide education and awareness through survivorship resources, and require study of the existing reimbursement landscape and development of an alternative payment model, among many other things.
In closing, Congresswoman Wasserman Schultz acknowledged the challenging work that lies ahead to pass this legislation and called on all members of the cancer community to lend their voices to this collective effort to improve the quality of life and quality of care for cancer survivors.
Mid-Term Election Update: What to Expect for the Future of Health Policy
Panel Discussion

McDermott+Consulting
Shelagh Foster, JD
Polsinelli
Lydia Isaac, PhD, MSc
National Urban League
Polsinelli
Rodney Whitlock, PhD
McDermott+Consulting
Shelley Fuld Nasso
National Coalition for Cancer Survivorship
Summary
Panel Speakers
Patricia Ganz, MD – Palliative Care is Survivorship Care
UCLA School of Medicine
2022 Ellen L. Stovall Health Care Professional Award Winner
Summary
 In this session, NCCS founding member and Stovall Award winner, Dr. Patricia Ganz, presented the many reasons why palliative care is integral to survivorship care. From the beginning of her career, Dr.Ganz recognized the importance of delivering palliative care to cancer patients from the time of diagnosis rather than waiting until the last few weeks of life to enhance their quality of life. She stressed that services such as care planning, palliative care, psychosocial support, prevention and management of long-term and late effects, and family caregiver support should be delivered to patients and their families throughout the entire continuum of care.
In this session, NCCS founding member and Stovall Award winner, Dr. Patricia Ganz, presented the many reasons why palliative care is integral to survivorship care. From the beginning of her career, Dr.Ganz recognized the importance of delivering palliative care to cancer patients from the time of diagnosis rather than waiting until the last few weeks of life to enhance their quality of life. She stressed that services such as care planning, palliative care, psychosocial support, prevention and management of long-term and late effects, and family caregiver support should be delivered to patients and their families throughout the entire continuum of care.
In her presentation, Dr. Ganz shared the three “p’s” of survivor care: palliation, prevention, and health promotion. She emphasized the need to educate professional and patient communities so they understand the purpose and benefits of palliative care and cultivate specialists’ interest in palliative care of cancer survivors. She acknowledged the importance of secondary prevention of cancer in survivors, noting that 15% of new cancer diagnoses are in individuals who have had cancer previously. Additionally, she highlighted how critical lifestyle modifications and surveillance can be to reduce the risk of a second cancer and other chronic conditions.
Patricia Ganz, MD – Stovall Award Video
Alicia Staley – Survivorship and Advocacy
VP, Patient Engagement – Medidata
2022 Ellen L. Stovall Patient Advocate Award Winner
Summary
 In a personal interview, Alicia Staley, three-time cancer survivor, Stovall Award winner, and experienced patient advocate, traced her advocacy journey, acknowledging how her advocacy has helped support her as a survivor while her survivorship has helped drive and energize her advocacy. Diagnosed with cancer for the first time at just 19 years old, she never anticipated that she would become involved in cancer advocacy. However, after she was personally confronted with the complex and overwhelming environment that cancer survivors face, she openly questioned the lack of innovation in health care and was invited to join her first patient advisory board. She never looked back.
In a personal interview, Alicia Staley, three-time cancer survivor, Stovall Award winner, and experienced patient advocate, traced her advocacy journey, acknowledging how her advocacy has helped support her as a survivor while her survivorship has helped drive and energize her advocacy. Diagnosed with cancer for the first time at just 19 years old, she never anticipated that she would become involved in cancer advocacy. However, after she was personally confronted with the complex and overwhelming environment that cancer survivors face, she openly questioned the lack of innovation in health care and was invited to join her first patient advisory board. She never looked back.
An early adopter of Twitter, she shared how social media helped her find other people like her, which in turn inspired her to create #BCSM, a global breast cancer community. She shared how her advocacy led to a career change, as she now works to bring patient insights to clinical trial design, centering clinical trials around the needs and experience of the patient. For example, she has recently worked to encourage industry stakeholders to reconsider their approach to sharing informed consent with patients, urging them to use digital platforms as educational tools to deliver complex information.
Alicia Staley – Stovall Award Video
Medical Debt for Cancer Survivors
Panel Discussion

A discussion around Diagnosis: Debt – A reporting partnership between Kaiser Health News and National Public Radio, “exploring the scale, impact, and causes of medical debt in America.”
Kaiser Health News
Kristie Fields
PinkSlayer
Lauren Ghazal, PhD
University of Michigan
MD Anderson Cancer Center
Shelley Fuld Nasso
National Coalition for Cancer Survivorship
Summary
Panel Speakers

Noam N. Levey
Noam N. Levey, Senior Correspondent, joined KHN in January 2021 after 17 years at the Los Angeles Times, the last 12 as the paper’s national health care reporter based in Washington, D.C. Noam has reported on health care issues from more than three dozen states and four continents and won numerous honors, including the prestigious NIHCM award for his 2019 series “Inside America’s High-Deductible Revolution.” He has also been published in Health Affairs, JAMA, and The Milbank Quarterly.
Noam started his career at newspapers in Duluth, Minnesota; Montgomery, Alabama; and the United Arab Emirates. Before his stint at the L.A. Times, he was an investigative reporter for the San Jose Mercury News. Noam has a degree in history and Near Eastern studies from Princeton University.

Kristie Fields
Kristie Fields is a breast and colon cancer survivor. After battling cancer, Kristie received her BS in Business Management and a Master’s in health science. Her goal was to be an administrator at a local hospitals or cancer centers. However, she was not able to get a fellowship because of COVID. Kristie then completed paperwork to become a nonprofit, advocating for at-risk populations and veterans. She goes into neighborhoods to educate people about how to communicate with health care professionals. She provides training sessions, motivational speaking, and navigates clients through the health care system. Kristie is a veteran and provides training programs for veterans as well. She teaches others how to get through their diagnosis and thrive. She would like to connect with CPAT participants to learn how to expand her organization and do more for her community.
Visit the website of Kristie’s non-profit, Pinkslayer.

Lauren Ghazal, PhD, FNP-BC
Lauren Ghazal, PhD, FNP-BC, is a family nurse practitioner and post-doctoral research fellow at the University of Michigan – Ann Arbor. She is affiliated with the Center for Improving Patient and Population Health at the School of Nursing and the Rogel Cancer Center. Dr. Ghazal completed her PhD at the Rory Meyers College of Nursing at New York University, where she was a T42 pre-doctoral fellow in Occupational and Environmental Health and received grant support from the National Institutes for Occupational Safety and Health. Her dissertation focused on work-related challenges and financial toxicity in adolescents and young adult (AYA) cancer survivors. Her broader program of research builds on her background in economics, clinical, and personal experiences to address cancer survivorship disparities in adolescents and young adults.
Ya-Chen Tina Shih, PhD
Ya-Chen Tina Shih, PhD, is professor and Chief of Section of Cancer Economics and Policy, Department of Health Services Research at the University of Texas MD Anderson Cancer Center. Her research applies health econometric methods to study technology diffusion in cancer and modeling methods to evaluate cost-effectiveness of screening strategies. Dr. Shih is associate editor of Journal of the National Cancer Institute and is a member of the American Cancer Society Guidelines Development Workgroup.
Closing Keynote: Monica Bertagnolli, MD
Director, National Cancer Institute
“Survivors are not just the products of their diagnosis. They are not what we have taken or what cancer has taken from them. They may be forever changed, but they are certainly whole.”
Summary
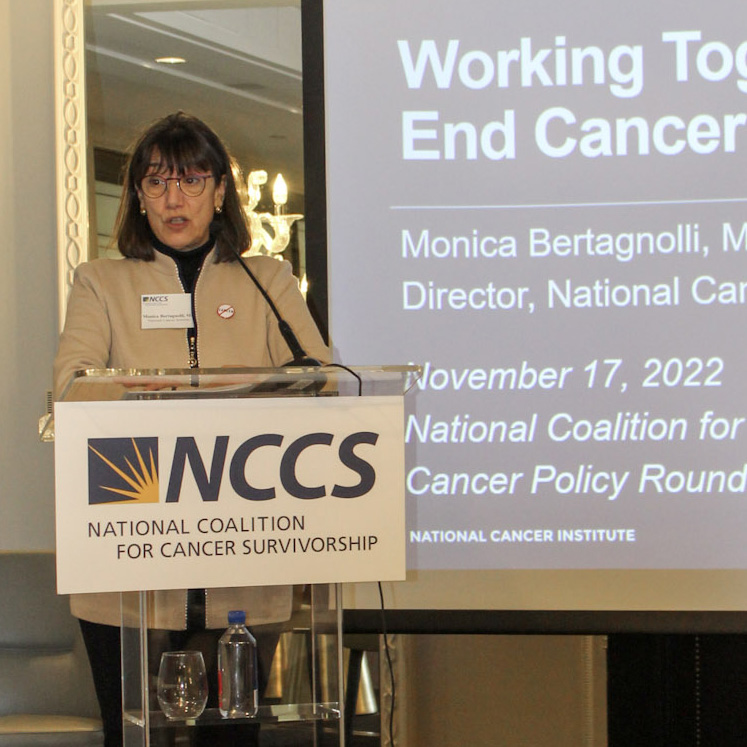 We were honored to have Dr. Monica Bertagnolli, National Cancer Institute’s (NCI) new Director, attend the Fall 2022 Cancer Policy Roundtable and deliver the closing keynote. As a surgeon and oncologist for over 30 years, she worked with cancer survivors every day and understands that every survivor’s experience is unique. She stressed throughout her speech the importance of and her dedication to keeping survivors front and center, by listening to and engaging them, when establishing NCI’s research priorities and focus.
We were honored to have Dr. Monica Bertagnolli, National Cancer Institute’s (NCI) new Director, attend the Fall 2022 Cancer Policy Roundtable and deliver the closing keynote. As a surgeon and oncologist for over 30 years, she worked with cancer survivors every day and understands that every survivor’s experience is unique. She stressed throughout her speech the importance of and her dedication to keeping survivors front and center, by listening to and engaging them, when establishing NCI’s research priorities and focus.
Dr. Bertagnolli celebrated the progress that has been made but acknowledged that many challenges remain for patients and survivors in the cancer journey. She affirmed NCI’s commitment to improving care and quality of life for survivors through a broad range of research focused on, for example, disparities in childhood cancer, survivor outcomes, the impact of familial, socioeconomic, and other factors on health outcomes, and the development of targeted interventions to help reduce the burden of cancer for young survivors. She called for renewed focus on disparities in care for survivors, stressing the need to better understand where disparities are, why they exist, and how to eliminate them. This understanding, she said, is critical to ending cancer as we know it.
Cancer Policy Roundtable 2022 Sponsors











 Kristie Fields, founder of the cancer nonprofit PinkSlayer and member of NCCS Cancer Policy and Advocacy Team, shared her valuable insights as a cancer survivor, discussing her personal survivorship journey and the importance of family. When she was diagnosed with cancer after losing her job and experienced financial hardships first-hand, her family played a large role in providing financial and emotional support and helping her care for her children. Cancer patients, she said, “Shouldn’t have to choose to go to treatment or eat or feed your family – that should be a no brainer.” Her experience led her to begin buying groceries, gas, and other necessities for cancer patients in her community. In 2016, she officially started her own cancer nonprofit to provide navigation, education, and support to cancer patients and their families.
Kristie Fields, founder of the cancer nonprofit PinkSlayer and member of NCCS Cancer Policy and Advocacy Team, shared her valuable insights as a cancer survivor, discussing her personal survivorship journey and the importance of family. When she was diagnosed with cancer after losing her job and experienced financial hardships first-hand, her family played a large role in providing financial and emotional support and helping her care for her children. Cancer patients, she said, “Shouldn’t have to choose to go to treatment or eat or feed your family – that should be a no brainer.” Her experience led her to begin buying groceries, gas, and other necessities for cancer patients in her community. In 2016, she officially started her own cancer nonprofit to provide navigation, education, and support to cancer patients and their families.

